Psychotic disorders can fundamentally shift a person’s grip on reality, creating challenges that ripple through families. When a loved one is battling a psychotic disorder, parents often feel an overwhelming mix of confusion, fear, and grief. For families facing the challenges of children struggling with addiction alongside psychotic disorders, the journey can feel particularly isolating. At Mothers Against Addiction , we know how crucial it is to provide a compassionate community where parents can share their experiences, find support, and gain hope.
In this article, we’ll delve into seven psychotic disorders that are known to dramatically alter how individuals perceive reality. Understanding these conditions and their implications can empower parents to approach their child’s struggles with empathy and effective strategies.

7 Psychotic Disorders that Change Reality Forever
Psychotic disorders manifest in various ways, and while they can be distressing, insight into their nature can help families navigate the tumultuous waters of recovery.

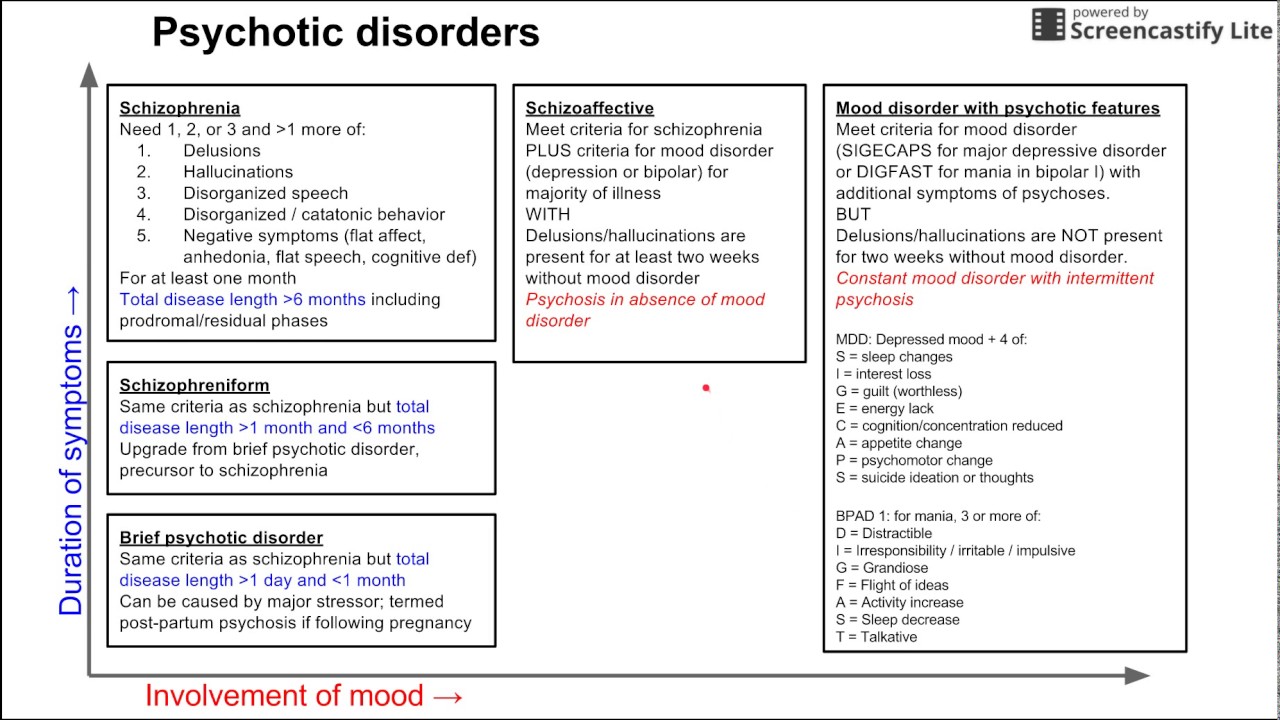
1. Schizophrenia
Schizophrenia is perhaps the most recognized of the psychotic disorders. It often shows up with hallucinations and delusions, which can lead to significant difficulties in daily life. Individuals may hear voices that others can’t, causing severe distress and impairing their ability to function. This disorder typically makes its appearance in late adolescence or early adulthood, fundamentally impacting relationships and the ability to engage in meaningful activities. Some people may even experience alarming thoughts of suicidality, highlighting the urgency for supportive networks.
When a parent sees their child struggling with schizophrenia symptoms, it can leave them feeling helpless. The unpredictability of this condition may push families to the brink as they seek effective treatment paths. Fostering open lines of communication about this disorder is vital for families who need to understand and support their loved ones through this profound challenge.
2. Schizoaffective Disorder
Schizoaffective disorder is a mix of schizophrenia and mood disorders. Patients endure psychotic symptoms along with emotional disturbances like depression or mania. It can lead to spontaneous mood swings that complicate the treatment process. Many individuals may turn to substances as a form of self-medication, grappling with alcoholism symptoms as they search for relief.
Parents must understand that this intertwining of conditions not only affects the individual but exerts stress on family dynamics. It’s essential for families to remain patient and educate themselves on the complexities of this disorder, fostering a healthy environment that embraces recovery.
3. Bipolar Disorder with Psychotic Features
Bipolar disorder can be a rollercoaster, marked by extreme mood swings. When it carries psychotic features, individuals may face hallucinations or delusions during manic or depressive episodes. An example could be someone believing they possess superhuman powers while in a manic state, only to spiral into paranoia when depressed. This disconnection from reality can lead to feelings of despair and sometimes even suicidality.
It’s crucial for parents to recognize bipolar symptoms early on. By identifying these patterns, families can work directly with healthcare professionals to create a detailed plan that addresses both the mood disorder and the underlying psychotic features, ultimately supporting the individual’s journey toward stability.
4. Psychotic Depression
Psychotic depression, unlike standard depression, adds a layer of complexity with its psychotic features. Here, patients may think they are responsible for distressing events or harbor feelings of worthlessness, leading to increased risks of self-harm or suicidality. These hallucinations often echo their feelings of despair, amplifying their emotional turmoil.
For families coping with this disorder, it’s vital to foster an environment of understanding and connection. Strengthening family bonds and nurturing open dialogues can lead to better outcomes and a shared commitment to wellness.
5. Alcohol-Induced Psychotic Disorder
In cases of heavy alcohol consumption, individuals may encounter hallucinations and delusions, often mimicking the troubling experiences associated with schizophrenia. This disorder typically emerges during or after excessive drinking, presenting a challenge for families who feel helpless in the face of addiction.
The long-term implications of alcohol use can escalate into alcohol-induced dementia, complicating recovery and rehabilitation. For parents, navigating their child’s struggles with addiction intertwined with psychosis often brings feelings of frustration and despair. Seeking intervention and support through resources tailored for families battling addiction is essential in these situations.
6. Brief Psychotic Disorder
Brief psychotic disorder may appear suddenly in response to intense stress or trauma. Its symptoms typically last less than a month, leaving individuals puzzled about their reality. While it may resolve without formal treatment, the aftermath can still create lingering effects on mental health and relationships.
Families faced with this disorder might feel relief as symptoms subside. However, ongoing care with therapists or support groups is vital to ensuring individuals can process their experiences and continue on their healing journey.
7. Delusional Disorder
Delusional disorder is marked by deeply held false beliefs that disrupt daily functioning. These fixed beliefs can lead to social withdrawal, increasing feelings of isolation and anxiety. It can disrupt personal lives and wreak havoc on professional relationships, making it hard for the individual to connect.
For families, understanding the nature of delimiting beliefs is crucial to creating supportive environments. Open conversations and effective strategies can help in managing relationships with loved ones battling this debilitating disorder.
The Intersection of Psychotic Disorders and Substance Abuse
There’s a significant overlap between psychotic disorders and substance abuse, particularly concerning alcohol. Those battling schizophrenia often find themselves facing alcoholism symptoms, which can exacerbate cognitive impairments. Understanding the interplay between these issues is crucial for developing an effective treatment plan.
Families must address both the mental health needs and potential substance misuse in their loved ones. Taking proactive steps through community resources and structured support systems can help facilitate healing and recovery.
Understanding Mood Disorders’ Role in Psychotic Events
Mood disorders can set the stage for psychotic symptoms to emerge. Awareness of this relationship can pave the way for early interventions, preventing more severe complications. Recognizing bipolar symptoms alongside psychosis can be a starting point for families to take action.
When parents are educated about these connections, they can work with professionals to develop holistic treatment approaches. This comprehensive understanding fosters a sense of empowerment that can be incredibly beneficial for families navigating these turbulent times.

Innovative Strategies for Supporting Affected Families
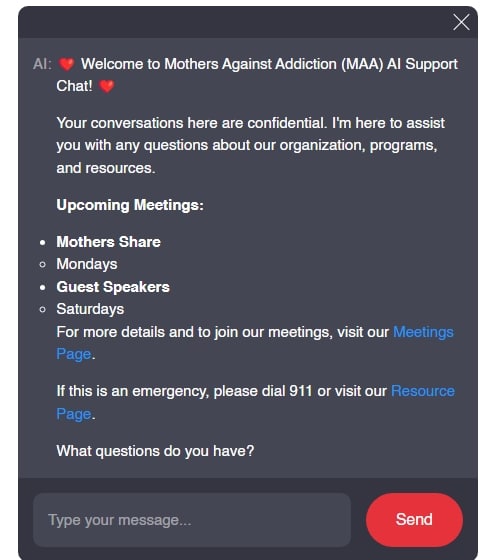
Supporting families impacted by psychotic disorders requires a multi-faceted approach. It’s essential to offer educational programs and resources focused on the specific challenges posed by these conditions. Community support groups, such as those organized by Mothers Against Addiction, serve as a lifeline for parents, allowing them to share their experiences and learn from one another.
Peer support can build resilience, offering hope and camaraderie in almost unbearable circumstances. Families sharing strategies and coping mechanisms creates a sense of community that empowers individuals to face their challenges with renewed strength.
The journey through psychotic disorders isn’t easy, but with awareness, community support, and open communication, families can navigate the complexities of reality-altering conditions. Standing together, we can foster understanding and create environments where healing is possible, enabling families to withstand the challenges posed by psychotic disorders and addiction.
Together, let’s play our part in supporting those we love, offering compassion and understanding in the fight against addiction and its associated struggles. To learn more about coping skills for anxiety and how to support your loved ones effectively, visit This helpful resource.
In the end, we must remember, it’s okay to seek help. We’re all in this together. Let’s keep the dialogue open, continue learning, and support each other as we navigate the difficult terrains brought on by psychotic disorders.
The Intriguing World of Psychotic Disorders
Psychotic disorders can be a tough topic to digest, but they encapsulate some fascinating trivia worth exploring. Did you know that psychotic disorders can cause a person to lose touch with reality? This disconnect can often lead to symptoms like hallucinations and delusions. For instance, people with schizophrenia may hear voices that others can’t, making everyday life challenging. Speaking of challenging, if you’re curious about the science behind mental health, the med definition might provide some clarity.
Everyday Insights into Psychotic Disorders
Speaking of reality checks, many movies tackle themes of psychotic disorders, providing a dramatized glimpse into these struggles. One such flick is “It Ends With Us,” which addresses emotional and psychological challenges faced by individuals, illustrated well in the film’s trailer. Also, interestingly enough, some individuals report altered perceptions after consuming hallucinogens, leading to the question: How long Does it take acid To kick in? That’s another layer of complexity on the subject of altered reality and mental health.
The Broader Implications
Research into psychotic disorders often involves extensive lab testing to develop new therapies and understand these conditions better. And while we’re on the topic of testing, consider how the arts mirror these experiences. Shows and films can serve as a mirror into the emotional turbulence of psychotic disorders. For instance, the film Longhorns creatively tackles themes of emotional conflict and social dynamics in contexts that could provoke deeper considerations surrounding mental health. In addition to entertainment, it can provoke thought about societal perceptions of mental illnesses.
Understanding psychotic disorders entails looking beyond the symptoms into the human experience. From hallucinations that might make one feel like they’re living in a volcanic eruption, as portrayed through artistic interpretations, to personal stories that reveal the impact of these disorders, every narrative holds weight. So the next time you explore films or literature, think of how they may resonate with realities shaped by psychotic disorders, much like the artistry in a volcano cast. Insight into these narratives could foster understanding or even empathy for those facing such challenges.